Game-Changing Medicare Part D Reform Will Be Possible With The Inflation Reduction Act
"Right now we pay a lot of money, regardless of whether a drug has clinical benefits for patients." - Stacie B. Dusetzina, Ph.D
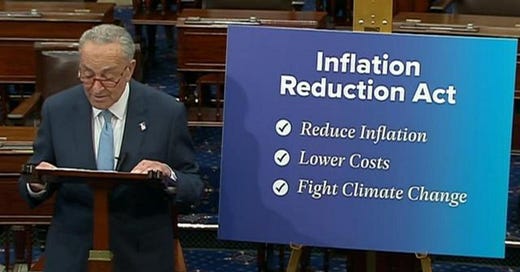
TL;DR: The Inflation Reduction Act was passed in the Senate on August 7th, 2022 through a process called reconciliation. The Inflation Reduction Act allows for some key policy changes that will have a significant impact on reducing medication prices for many patients on Medicare, policy changes which Dr. Stacie B. Dusetzina strongly advocates for. Dr. Dusetzina sees the Center for Medicare and Medicaid Innovation continuing to offer excellent opportunities for the creation of novel pricing strategies (CMMI). Dr. Dusetzina wants to see a shift in the way that drug costs are determined—one that bases rates on the value that the drug offers.
Terminology:
Reconciliation: allows Congress to pass legislation on taxes, spending, and the debt ceiling with just a majority in the Senate (51 votes, or 50 if the vice president breaks a tie), avoiding the possibility of a filibuster, which needs 60 votes to be overridden.
Pharmacy benefit managers (PBMs) are paid third-party administrators of prescription drug coverage for insurers and employers.
Medicare: Medicare is the US’s health insurance program for people age 65 or older. Certain people younger than age 65 can qualify for Medicare too, including those with disabilities and those who have permanent kidney failure.
Medicare Part D: Medicare beneficiaries have the option to sign up for the outpatient prescription medication benefit, which is offered through private plans that have received federal approval.
The Problem
The cost of medications is well-known to be high in the US. Insulin is the most frequently cited example. Based upon the Health Affairs paper, "catastrophic" levels of insulin spending are experienced by 14% of Americans who use insulin. This indicates that after paying for food and housing, these patients spend at least 40% of their income on insulin.
The Inflation Reduction Act, which was passed in the Senate on August 7th, 2022, through a process known as reconciliation, provides a ray of hope in the face of rising medication prices. The Inflation Reduction Act allows for some key policy changes which will have a significant impact on reducing medication prices for Medicare patients enrolled in Part D programs. Including the ability for Medicare to negotiate medication prices directly with drug makers.
In order to better understand the development of drug pricing in the US, I had the opportunity to ask some questions to Stacie B. Dusetzina, Ph.D., an associate professor in the Department of Health Policy and an Ingram Associate Professor of Cancer Research at Vanderbilt. Dr. Dusetzina is a health care researcher whose work focuses on quantifying and analyzing pharmaceutical use and expenditures at the population level in the US.
*Questions were asked prior to the Senate's passing of the Inflation Reduction Act.
Misunderstandings in Pricing
EB [Evan Brociner]: From your experience, what are some of the most misunderstood reasons people think medication pricing is so high in the U.S. that you would like to clarify?
SD [Stacie Dusetzina]: One misunderstanding is that the price of a drug reflects how much it costs to develop the drug. In fact, companies set their prices based on how much money they think they can get (“what the market will bear”). Even if it was less expensive to make a drug, it is unlikely that it would lower drug prices.
The role of pharmacy benefits managers is also really misunderstood. They are typically framed as being a “middle man” in the negotiations between insurers and manufacturers. In fact, pharmacy benefits managers are how we negotiate for lower drug prices today. There are debates about whether they make too much money for doing this work, but if they didn’t exist in our current system, health plans, employers, and patients would likely pay more for their drugs.
Pharmacy benefit managers
Pharmacy benefit managers (PBMs) are paid third-party administrators of prescription drug coverage for insurers and employers. PBMs are used by commercial insurers, in Medicare for its Part D benefit, and in the Medicaid program—particularly by Medicaid managed care organizations.
PBMs have a lot of power over what consumers pay for drugs. And a consolidation of the industry over the past several years has made that even more true. Now just three dominate: CVS Caremark, Express Scripts, and OptumRx. In total, they cover more than 150 million people.
A big part of their job is to bring down the cost of medication for employers. They do this by negotiating with pharmaceutical companies for rebates. Sometimes the PBMs pocket a portion of the rebate and pass another portion to the insurance company or the employer.
As Dr. Dusetzina mentioned, there is a lot of controversy regarding whether PBMs make too much money. As well, there is controversy surrounding whether PBMs increase the prices for medications for consumers who go through their insurance for their medication. An argument that people have for the benefit of PBMs is that PBMs serve as a barrier between pharmaceutical companies charging even more for medications.
Medicare Part D
Medicare Part D is a significant area where drug costs can be reduced for many Americans. Of the more than 62 million individuals covered by Medicare in 2021, 48 million are enrolled in Part D programs. Medicare beneficiaries have the option to sign up for the outpatient prescription medication benefit, which is offered through private plans that have received federal approval.
A Medicare Advantage prescription drug plan (MA-PD), primarily HMOs and PPOs, offers full Medicare benefits, including prescription medications, or a stand-alone prescription drug plan (PDP) to augment regular Medicare.
EB: With recent talk from Democrats about Medicare drug prices, how do you hope that the much-needed reform in Medicare Part D identified in your recent Health Affairs paper will be incorporated into upcoming legislation?
SD: Democrats are attempting to move Part D reform through a process called reconciliation. If successful, they would be implementing some substantial changes to the Medicare Part D program, including changing how the program pays for drugs, and limiting annual out-of-pocket spending for beneficiaries to $2,000. This legislation also introduces drug price negotiation into Medicare, which could help to address drug spending more broadly.
For a more detailed understanding of the Inflation Reduction Act’s impact on Medicare Part D, here and here are great articles.
More Congressional Policy?
While the Inflation Reduction Act will have a significant impact on Medicare Part D, should we rely on Congress to have the answers to all of Medicare Part D's problems?
EB: You mention in your paper here, for example, proposing policy improvement. Do you have any lessons that you have learned from influencing and trying to apply policy changes to legislation?
SD: Even if the Democrats are successful at passing Medicare Part D policy reforms, there are other opportunities to consider how to make the benefit better for patients. For example, the Center for Medicare and Medicaid Innovation (CMMI) could run a demonstration project to try out different payment arrangements for high-cost drugs to see which options work best for helping patients to start and stay on their treatments.
Current Opportunities
EB: The Mark Cuban Cost Plus Drugs Company (MCCPDC) seems to be a great way to reduce medication pricing. Are there other companies taking new directions on medication pricing that you are encouraged by?
SD: Yes. CivicaRx is another interesting company that has been working to introduce drugs into the market that are either over-priced or in shortage. https://civicarx.org/ They are also working to produce a low-cost insulin product. Another company of interest is EQRx - they are developing head-to-head competitors for brand-name products. Instead of focusing on producing generics, they want to make brand-name drugs cheaper by competing on price. https://www.eqrx.com/ Finally, Blueberry Pharmacy (https://blueberrypharmacy.com/) is a brick-and-mortar version of Mark Cuban Cost Plus Drugs Company. They are a retail pharmacy in Pennsylvania that has focused on providing low cost drugs to their patients.
The Mark Cuban Cost Plus Drugs Company created its own PBM in late 2021 and has committed to being open and honest with its associates about the prices it pays for prescription drugs. It aims to completely do away with the conventional PBM model.
Longer-Term Solutions
EB: What do you hope the future of medication pricing will look like in the U.S., and what do you think the biggest challenges will be?
SD: I would like to see pricing reflect the benefit of the drugs for patients. Right now we pay a lot of money, regardless of whether a drug has clinical benefits for patients. The payment is tied to how competitive the market is (how many treatment options the patient has) and not tied to how much a drug improves outcomes. I believe we need to pay generously for drugs that have a lot of benefit and pay much less for drugs that have limited benefit. If we do this, I think we will incentivize innovation that truly benefits patients. The biggest challenge to this is the industry’s influence over Congress.
I'm looking forward to seeing the impact the Inflation Reduction Act has on improving medication pricing for the 48 million Americans who are Medicare beneficiaries and enrolled in Part D. This is one of the largest and best changes to healthcare since the passing of the Affordable Care Act.
Also, I'm hoping that more companies will introduce innovative methods for setting drug prices based on value. Additionally, I want to dig deeper into the controversy PBMs have on medication pricing, specifically their potential role in influencing legislation and viewpoints from experts on what they would like the future of PBMs to be.
If there are any unique experiences that you have seen that have had an impact on lowering the cost of medications, particularly from the viewpoint of PBMs and value-based pricing efforts, I would love to hear from you.
I’ve got a lot more coming this year from The Future As It Should Be. I always welcome ideas for interviews or topics you’d love for me to cover, so reach out anytime to @evanbrociner on Twitter.